NIR OCT has potential for skin cancer detection
Submitted by ianm on 1 October 2012 - 10:14am
Researchers from Medical University Vienna (MUW) in Austria and the Ludwig-Maximilians University in Munich, Germany, have used optical coherence tomography (OCT) to non-invasively map out the network of tiny blood vessels beneath the outer layer of patients’ skin, potentially revealing signs of disease. The researchers tested their system on a range of different skin conditions, including a healthy human palm, allergy-induced eczema on the forearm, dermatitis on the forehead, and two cases of basal cell carcinoma—the most common type of skin cancer—on the face. Compared to healthy skin, the network of vessels supplying blood to the tested lesions showed significantly altered patterns. “The condition of the vascular network carries important information on tissue health and its nutrition,” says Rainer Leitgeb, a researcher at MUW and the study’s principal investigator. “Currently, the value of this information is not utilised to its full extent.”
Ophthalmologists have used OCT since the 1990s to image different parts of the eye and the technology has recently attracted increased interest from dermatologists. OCT has many advantages over other imaging techniques: it is non-invasive and provides high-resolution images at high speed. OCT is typically used to show tissue structure, but it can also reveal the pattern of blood vessels, which carry important clues about disease, by capitalising on the unique optical properties of flowing blood cells.
The researchers at MUW are the first to use OCT to visualise the network of blood vessels in human skin that feed cancerous skin lesions. To maximise the quality of the images the team employed a high-tech laser light source developed by collaborators from the Ludwig-Maximilians University. The laser enabled unprecedented high-speed imaging and operated at a near infrared wavelength (1310 nm) that gave better penetration into skin tissue.
“High speed is of paramount importance in order to image lesions in vivo and in situ while minimising the effect of involuntary patient motion,” explains researcher Cedric Blatter of MUW. The device also shapes the light in a special way forming a Bessel beam, which can reform, or heal, its shape even if portions of it are blocked. The beam enabled the researchers to keep the images in focus across a depth range of approximately 1 mm.
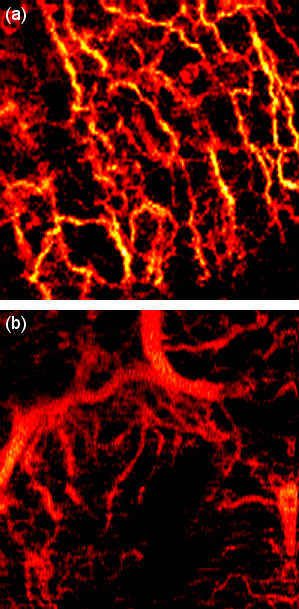
The team’s images of basal cell carcinoma showed a dense network of unorganised blood vessels, with large vessels abnormally close to the skin surface. The larger vessels branch into secondary vessels that supply blood to energy-hungry tumour regions. The images, together with information about blood flow rates and tissue structure, could yield important insights into the metabolic demands of tumours during different growth stages.
The imaging system shows the most promise for clinical application in the diagnosis and treatment of skin cancer, the researchers believe. “We hope that improved in-depth diagnosis of tissue alterations due to disease might help to reduce the number of biopsies by providing better guidance,” says Leitgeb. The system could also be used by doctors to assess how quickly a tumour is likely to grow and spread, as well as to monitor the effectiveness of treatments such as topical chemotherapy. “Treatment monitoring may also be expanded toward inflammatory and auto-immune related dermatological conditions,” Blatter notes.
Going forward, the researchers would like to increase the field of view of the device so that they can image the full lesion along with its border to healthy tissue. They are also working on speeding up the post-processing of the optical signal to enable live vasculature display, and improving the portability of the system, which currently occupies an area about half the size of an office desk. “We believe that in the future our method will help to simplify non-invasive dermatological in vivo diagnostics and allow for in-depth treatment monitoring,” says Blatter.
The research is reported in Biomedical Optics Express, doi: http://dx.doi.org/10.1364/BOE.3.002636.